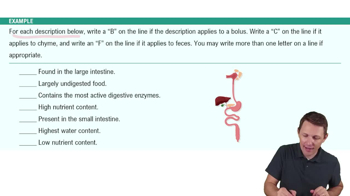
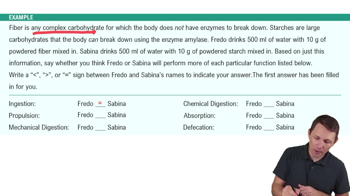
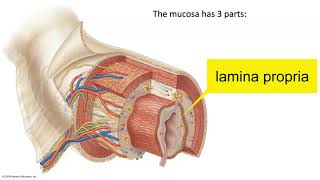
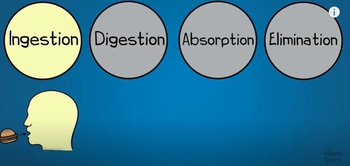
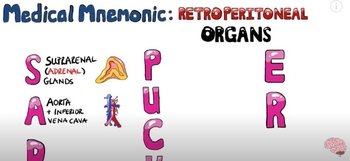
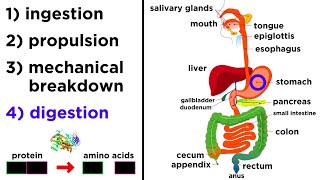
The digestive system consists of the gastrointestinal tract, or alimentary canal, and accessory digestive organs. Food enters the tract at the mouth and is processed by the organs. The contents that leave the system at the end of the tract are primarily undigested food. Your goals for learning are To identify the organs and sphincters of the gastrointestinal tract. To describe the structure of the wall of the gastrointestinal tract. To identify the accessory organs of the digestive system. To state a simplified function for each organ. Here's what you need to know That mucous membranes line body cavities that are open to the outside. The histological makeup of mucous membranes. The types of epithelial tissues and their functions. The histological organization of the four-layered wall in the GI tract is similar from the stomach to the last portion of the anal canal. Throughout the tract, modifications of the histological organization serve regional functions. Let’s begin with the small intestine. We will illustrate the histological organization using the wall of the small intestine. The villi, microvilli, and intestinal crypts are specific modifications of the small intestine. We will describe other regional modifications as we move through the tract. Let’s begin with the mucosa. An epithelium, made up of columnar cells, forms the inner or luminal boundary of the tract. The lamina propria, a connective tissue layer, underlies the epithelium and carries blood and lymph vessels. A thin sheet of smooth muscle, the muscularis mucosae, forms the deep boundary of this layer. Functions of the GI epithelium include Secretions of substances used in digestion Absorption of the digested products Goblet cells are found in the epithelium. Goblet cells secrete mucus. Other epithelial cells secrete fluids, such as acid in the stomach and water and salts in the small intestine. Secretory products are released into the lumen. Then, there are enteroendocrine cells. The hormones of the GI system are produced and secreted by individual mucosal cells called enteroendocrine cells. They are present over a large area. Stimuli for release are in the lumen or near the basal surface of the cells. Note that hormones are released into the interstitial fluid to enter capillaries of the lamina propria. Hormones are not released into the lumen of the GI tract. Nutrients are absorbed across a single layer of cells into blood capillaries or lymph vessels called lacteals. As we leave the mucosa, note that there are stem cells present throughout the GI tract that divide continuously to replace epithelial cells that are regularly shed. A new epithelium is produced every three to six days. Now, let’s discuss the muscularis mucosae. This thin muscle, with inner circular fibers and outer longitudinal fibers, moves the mucosa. These movements alter mucosal folds and move the villi to aid digestion and absorption. Then, there is the submucosa. The submucosa is loose connective tissue that carries blood and lymph vessels. At its deep boundary lies a network of intrinsic neurons, called the submucosal plexus that serves the digestive system. Next is the muscularis externa. The muscular portion of the wall contains two layers of smooth muscle. The innermost layer is circular while the outer layer is longitudinal. These muscles produce waves of muscular contraction known as peristalsis, and oscillatory movements of the intestines known as segmentation. Tucked between the smooth muscle layers lies another network of intrinsic neurons called the myenteric plexus. It is richly interconnected with the submucosal plexus. Together they form the enteric nervous system that serves the gut. Finally, there is the serosa. A serous membrane covers the external surface of the digestive tract that lies inside the peritoneal cavity. Its presence reduces friction as gastrointestinal organs fill and empty during digestion. The gastrointestinal tract is a muscular tube that begins at the mouth, or the oral cavity, and ends at the anus. Accessory organs include the teeth, tongue, gallbladder, and digestive glands. Let’s begin with the mouth. Food enters the GI tract through the mouth. Mechanical action of teeth and tongue break food apart and mix it with saliva. A chewed portion of food called a bolus is separated and swallowed. The epithelium, lining the mouth and pharynx, is stratified squamous. It provides protection against abrasion and high temperatures. The epithelium covering the hard palette and dorsal surface of the tongue is keratinized. Then, there is the esophagus. The esophagus has no digestive or absorptive functions. It is simply a conduit that conveys food from the pharynx to the stomach. The esophagus passes through the diaphragm at the esophageal hiatus. The upper third of the esophagus is striated muscle, the middle third is a mixture of striated and smooth muscle, and the lower third is smooth muscle. Like the mouth and pharynx, the lining is stratified squamous epithelium. Now, let’s move to the stomach. The stomach expands to store ingested food. Its movements pulverize lumps and mix stomach secretions with the food. Acidic gastric juice digests cells, tissues and some macromolecules. Partially digested food is called chyme. The stomach has four regions; the cardia, fundus, body, and pyloric region. The antrum is the largest part of the pyloric region and the pylorus is the constricted terminal portion. The empty stomach is flat with a volume of about 50 ml. Its interior is thrown into folds called rugae. The rugae flatten out as the fundus and body distend to accommodate a meal. The stomach can hold about 1 litre of food with little change in internal pressure. Pressure rises as the stomach distends further to accommodate upto 4 litres of food. In addition to the circular and longitudinal muscle layers of the GI tract, the stomach has an inner oblique layer. Muscles are thin in the fundus and body and produce only weak contractions. Gastric muscles increase in thickness in the pyloric region. Strong contractions in the pyloric region are important for mixing ingested food with gastric juice and emptying chyme into the small intestine. Now we’ll move to the small intestine. Most digestion and absorption occur in the small intestine. The stomach delivers chyme to the small intestine in little squirts. The rate of delivery matches the processing capacity of the intestine. Juices in the small intestine neutralize the acidic chyme, restore normal osmolarity, and continue digestion of macromolecules. Breakdown products of macromolecules are absorbed across the intestinal epithelium into blood or lymph. The small intestine has three regions: duodenum, jejunum, and ileum. The duodenum is just 8 to 11 inches long. The total length of jejunum and ileum is 8 to 13 feet, the jejunum slightly shorter than the ileum. Next, let’s see the internal structures of the small intestine. The interior of the small intestine contains many permanent circular folds called plicae circulares. The duodenum has few folds. Its function is to neutralize chyme and render it ice osmotic. The number of folds is greatest in the jejunum where most absorption takes place. Plicae circulares increase the absorptive surface area of this organ. The plicae are covered with finger-like projections of the mucosa called villi,which also increase the absorptive surface area. Villi are longest in the jejunum, and shortest in the terminal ileum. Let’s learn more about villi. The columnar epithelial cells of the small intestine have many tiny projections on their luminal surface called microvilli that further increase the absorptive surface area. The surface is called a brush border because it resembles the bristles of a hairbrush. Let’s learn about the immune functions of the small intestine. The GI tract provides an entryway into the body for pathogens, as well as for food and drink. Cells throughout the upper GI tract secrete antimicrobial agents, and gastric acid renders chyme nearly sterile. Some intestinal villus cells secrete both antibacterial enzymes and immunoglobulins. In the distal ileum, there are lymphoid nodules in the connective tissue beneath the epithelium. Normal bacteria from the large intestine may enter the small intestine. Lymphocytes in the nodules prevent these bacteria from entering the bloodstream. Next, we’ll study the large intestine. The small intestine delivers chyme to the large intestine. Water and salts are absorbed from the chyme as it progresses through the large intestine. Bacteria normally present produce some vitamins that are also absorbed. The large intestine has subdivisions including: the cecum, appendix, colon (including the ascending, transverse, descending, and sigmoid colon), rectum, and anal canal. The outer longitudinal layer of the muscular wall is reduced to three bands called teniae coli. Contractions of the inner circular layer of muscle form the sac-like impermanent haustra. In the distal anal canal, the simple columnar epithelium that began in the stomach changes to stratified squamous. It protects underlying tissues from abrasion. The anus is the outlet of the GI tract. The feces eliminated from the GI tract are primarily indigestible food combined with bacteria, inorganic material, and sloughed off epithelial cells. Sphincters separate the organs of the GI tract. They control the entrance of food into the tract, control the progression of material along the tract, prevent reflux of material, and control the elimination of feces. This is the upper esophageal sphincter. The upper esophageal sphincter is a thick layer of circular muscle at the superior end of the esophagus. This sphincter is skeletal muscle, and when constricted it prevents air from entering the esophagus. Next is the lower esophageal sphincter. The lower esophageal sphincter, or gastroesophageal sphincter, is at the gastroesophageal junction. No thickened circular muscle is present. A zone of increased pressure, called a physiological sphincter, functions like a circular muscle. When constricted, the lower esophageal sphincter prevents reflux of gastric contents into the esophagus. This is the pyloric sphincter. The pylorus has thick muscular walls. The greatly thickened circular muscle is called the pyloric sphincter. It controls the rate of gastric emptying, hence the name pyloric, a Greek word meaning “gatekeeper.” This is the ileocecal sphincter. The ileocecal sphincter, or valve, separates the terminal ileum from the cecum. Distension of the terminal ileum opens the sphincter to permit the flow of chyme into the large intestine. Distension of the colon closes the sphincter preventing reflux into the ileum. Finally, the anal sphincters. There are two anal sphincter muscles. The circular smooth muscle of the anal canal thickens to form the internal anal sphincter. It is under involuntary control. Skeletal muscle surrounds the anal canal to form the external anal sphincter which is controlled voluntarily. Relaxation of both anal sphincters permits defecation. The salivary glands, liver, and pancreas produce secretions that are discharged into the lumen of the GI tract. These are the accessory glands. The salivary glands produce saliva that moistens ingested food, and cleanses and protects the mouth. The major digestive function of the liver is the production of bile. It is produced continuously by hepatocytes, and is stored and concentrated in the gallbladder. Bile is necessary for the digestion and absorption of fat. The exocrine pancreas produces digestive juice that contains enzymes to digest all major foodstuffs. It also produces bicarbonate to neutralize acidic chyme from the stomach. Here’s the summary of what we have covered The digestive system consists of a muscular tube and accessory organs. The wall of the GI tract from stomach to anus has four layers. The stomach stores and digests food. Most digestion and absorption occurs in the small intestine. Accessory glands produce juices that support digestion.
Table of contents
- 1. Introduction to Anatomy & Physiology5h 40m
- What is Anatomy & Physiology?20m
- Levels of Organization13m
- Variation in Anatomy & Physiology12m
- Introduction to Organ Systems27m
- Homeostasis9m
- Feedback Loops11m
- Feedback Loops: Negative Feedback19m
- Feedback Loops: Positive Feedback11m
- Anatomical Position7m
- Introduction to Directional Terms3m
- Directional Terms: Up and Down9m
- Directional Terms: Front and Back6m
- Directional Terms: Body Sides12m
- Directional Terms: Limbs6m
- Directional Terms: Depth Within the Body4m
- Introduction to Anatomical Terms for Body Regions3m
- Anatomical Terms for the Head and Neck8m
- Anatomical Terms for the Front of the Trunk8m
- Anatomical Terms for the Back9m
- Anatomical Terms for the Arm and Hand9m
- Anatomical Terms for the Leg and Foot15m
- Review- Using Anatomical Terms and Directions12m
- Abdominopelvic Quadrants and Regions19m
- Anatomical Planes & Sections17m
- Organization of the Body: Body Cavities13m
- Organization of the Body: Serous Membranes14m
- Organization of the Body: Serous Membrane Locations8m
- Organization of the Body: Thoracic Cavity8m
- Organization of the Body: Abdominopelvic Cavity12m
- 2. Cell Chemistry & Cell Components12h 37m
- Atoms- Smallest Unit of Matter57m
- Isotopes39m
- Introduction to Chemical Bonding19m
- Covalent Bonds40m
- Noncovalent Bonds5m
- Ionic Bonding37m
- Hydrogen Bonding19m
- Introduction to Water7m
- Properties of Water- Cohesion and Adhesion7m
- Properties of Water- Density8m
- Properties of Water- Thermal14m
- Properties of Water- The Universal Solvent17m
- Acids and Bases12m
- pH Scale21m
- Carbon8m
- Functional Groups9m
- Introduction to Biomolecules2m
- Monomers & Polymers11m
- Carbohydrates23m
- Proteins25m
- Nucleic Acids34m
- Lipids28m
- Microscopes10m
- Prokaryotic & Eukaryotic Cells26m
- Introduction to Eukaryotic Organelles16m
- Endomembrane System: Protein Secretion34m
- Endomembrane System: Digestive Organelles15m
- Mitochondria & Chloroplasts21m
- Endosymbiotic Theory10m
- Introduction to the Cytoskeleton10m
- Cell Junctions8m
- Biological Membranes10m
- Types of Membrane Proteins7m
- Concentration Gradients and Diffusion9m
- Introduction to Membrane Transport14m
- Passive vs. Active Transport13m
- Osmosis33m
- Simple and Facilitated Diffusion17m
- Active Transport30m
- Endocytosis and Exocytosis15m
- 3. Energy & Cell Processes10h 7m
- Introduction to Energy15m
- Laws of Thermodynamics15m
- Chemical Reactions9m
- ATP20m
- Enzymes14m
- Enzyme Activation Energy9m
- Enzyme Binding Factors9m
- Enzyme Inhibition10m
- Introduction to Metabolism8m
- Redox Reactions15m
- Introduction to Cellular Respiration22m
- Types of Phosphorylation11m
- Glycolysis19m
- Pyruvate Oxidation8m
- Krebs Cycle16m
- Electron Transport Chain14m
- Chemiosmosis7m
- Review of Aerobic Cellular Respiration19m
- Fermentation & Anaerobic Respiration23m
- Introduction to Cell Division22m
- Organization of DNA in the Cell17m
- Introduction to the Cell Cycle7m
- Interphase18m
- Phases of Mitosis48m
- Cytokinesis16m
- Cell Cycle Regulation18m
- Review of the Cell Cycle7m
- Cancer13m
- Introduction to DNA Replication22m
- DNA Repair7m
- Central Dogma7m
- Introduction to Transcription20m
- Steps of Transcription19m
- Genetic Code25m
- Introduction to Translation30m
- Steps of Translation23m
- Post-Translational Modification6m
- 4. Tissues & Histology10h 3m
- Introduction to Tissues & Histology16m
- Introduction to Epithelial Tissue24m
- Characteristics of Epithelial Tissue37m
- Structural Naming of Epithelial Tissue19m
- Simple Epithelial Tissues1h 2m
- Stratified Epithelial Tissues55m
- Identifying Types of Epithelial Tissue32m
- Glandular Epithelial Tissue26m
- Introduction to Connective Tissue36m
- Classes of Connective Tissue8m
- Introduction to Connective Tissue Proper40m
- Connective Tissue Proper: Loose Connective Tissue56m
- Connective Tissue Proper: Dense Connective Tissue49m
- Specialized Connective Tissue: Cartilage44m
- Specialized Connective Tissue: Bone12m
- Specialized Connective Tissue: Blood9m
- Introduction to Muscle Tissue7m
- Types of Muscle Tissue45m
- Introduction to Nervous Tissue8m
- Nervous Tissue: The Neuron8m
- 5. Integumentary System2h 20m
- 6. Bones & Skeletal Tissue2h 16m
- An Introduction to Bone and Skeletal Tissue18m
- Gross Anatomy of Bone: Compact and Spongy Bone7m
- Gross Anatomy of Bone: Periosteum and Endosteum11m
- Gross Anatomy of Bone: Bone Marrow8m
- Gross Anatomy of Bone: Short, Flat, and Irregular Bones5m
- Gross Anatomy of Bones - Structure of a Long Bone23m
- Microscopic Anatomy of Bones - Bone Matrix9m
- Microscopic Anatomy of Bones - Bone Cells25m
- Microscopic Anatomy of Bones - The Osteon17m
- Microscopic Anatomy of Bones - Trabeculae9m
- 7. The Skeletal System2h 35m
- 8. Joints2h 17m
- 9. Muscle Tissue2h 33m
- 10. Muscles1h 11m
- 11. Nervous Tissue and Nervous System1h 35m
- 12. The Central Nervous System1h 6m
- 13. The Peripheral Nervous System1h 26m
- Introduction to the Peripheral Nervous System5m
- Organization of Sensory Pathways16m
- Introduction to Sensory Receptors5m
- Sensory Receptor Classification by Modality6m
- Sensory Receptor Classification by Location8m
- Proprioceptors7m
- Adaptation of Sensory Receptors8m
- Introduction to Reflex Arcs13m
- Reflex Arcs15m
- 14. The Autonomic Nervous System1h 38m
- 15. The Special Senses2h 41m
- 16. The Endocrine System2h 48m
- 17. The Blood1h 22m
- 18. The Heart1h 42m
- 19. The Blood Vessels3h 35m
- 20. The Lymphatic System3h 16m
- 21. The Immune System14h 37m
- Introduction to the Immune System10m
- Introduction to Innate Immunity17m
- Introduction to First-Line Defenses5m
- Physical Barriers in First-Line Defenses: Skin13m
- Physical Barriers in First-Line Defenses: Mucous Membrane9m
- First-Line Defenses: Chemical Barriers24m
- First-Line Defenses: Normal Microbiota7m
- Introduction to Cells of the Immune System15m
- Cells of the Immune System: Granulocytes28m
- Cells of the Immune System: Agranulocytes26m
- Introduction to Cell Communication5m
- Cell Communication: Surface Receptors & Adhesion Molecules16m
- Cell Communication: Cytokines27m
- Pattern Recognition Receptors (PRRs)48m
- Introduction to the Complement System24m
- Activation Pathways of the Complement System23m
- Effects of the Complement System23m
- Review of the Complement System13m
- Phagocytosis17m
- Introduction to Inflammation18m
- Steps of the Inflammatory Response28m
- Fever8m
- Interferon Response25m
- Review Map of Innate Immunity
- Introduction to Adaptive Immunity32m
- Antigens12m
- Introduction to T Lymphocytes38m
- Major Histocompatibility Complex Molecules20m
- Activation of T Lymphocytes21m
- Functions of T Lymphocytes25m
- Review of Cytotoxic vs Helper T Cells13m
- Introduction to B Lymphocytes27m
- Antibodies14m
- Classes of Antibodies35m
- Outcomes of Antibody Binding to Antigen15m
- T Dependent & T Independent Antigens21m
- Clonal Selection20m
- Antibody Class Switching17m
- Affinity Maturation14m
- Primary and Secondary Response of Adaptive Immunity21m
- Immune Tolerance28m
- Regulatory T Cells10m
- Natural Killer Cells16m
- Review of Adaptive Immunity25m
- 22. The Respiratory System3h 20m
- 23. The Digestive System2h 5m
- 24. Metabolism and Nutrition4h 0m
- Essential Amino Acids5m
- Lipid Vitamins19m
- Cellular Respiration: Redox Reactions15m
- Introduction to Cellular Respiration22m
- Cellular Respiration: Types of Phosphorylation14m
- Cellular Respiration: Glycolysis19m
- Cellular Respiration: Pyruvate Oxidation8m
- Cellular Respiration: Krebs Cycle16m
- Cellular Respiration: Electron Transport Chain14m
- Cellular Respiration: Chemiosmosis7m
- Review of Aerobic Cellular Respiration18m
- Fermentation & Anaerobic Respiration23m
- Gluconeogenesis16m
- Fatty Acid Oxidation20m
- Amino Acid Oxidation17m
- 25. The Urinary System2h 39m
- 26. Fluid and Electrolyte Balance, Acid Base Balance Coming soon
- 27. The Reproductive System2h 5m
- 28. Human Development1h 21m
- 29. Heredity Coming soon
23. The Digestive System
Introduction to the Digestive System
Video duration:
15mPlay a video:
Related Videos
Related Practice