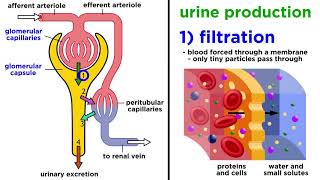
The urinary system rids the body of waste materials and controls the volume and composition of body fluids. Highly specialized cells in the kidneys are essential to these processes. Your goals for learning are: To review the anatomy of the urinary system, particularly the kidney. To examine the vascular and tubular portions of the nephron. To compare and contrast the specialized cells of the tubular epithelium. To review the unique structure of the juxtaglomerular apparatus. Here's what you need to know. The structural characteristics of epithelial cells. The urinary system is composed of paired kidneys and ureters, the urinary bladder, and the urethra. Urine is produced in the kidneys and then drains through the ureters to the urinary bladder, where the urine is stored. Urine is eliminated from the body through the urethra. Now let's take a closer look at a kidney's surrounding structures. Here we see that each bean-shaped kidney is embedded in the perirenal fat capsule. The kidneys are retroperitoneal, lying against the dorsal body wall in the upper abdomen. An adrenal gland which is part of the endocrine system lies on top of each kidney. Several structures enter or exit the concave surface of the kidney at the renal hilum, including the ureter and a renal vein which drains into the inferior vena cava. Let's learn more about the kidney's blood supply and see the underlying renal artery, after the left renal vein is removed. When the renal vein is removed and the kidney is shown in frontal section, you can see the deeper renal artery and its connection to the abdominal aorta. Branching from the renal artery are the segmental and interlobar arteries. Together these vessels provide the kidneys with a rich blood supply under high pressure that allows them to continuously filter and cleanse the blood. Now, let us take a closer look at a left kidney's internal structure. Internally, the human kidney is composed of three distinct regions: The first region is the outermost layer called the renal cortex. It contains about one million nephrons, the filtering units that form urine. There are two types of nephrons: cortical nephrons and juxtamedullary nephrons. Cortical nephrons lie largely with the cortex but their nephron loops dip into the medulla. Juxtamedullary nephrons have glomeruli that lie at the border of the cortex and the medulla and their nephron loops dip deeply into the medulla. The second region of the kidney is the middle layer called the renal medulla in which you can see the triangular renal pyramids. These pyramids look striated because of parallel bundles of ducts carrying urine from the nephrons. The areas between pyramids are the renal columns. They are extensions of the cortex that provide a route for the passage of blood vessels and nerves to and from the outer cortex. The third region of the kidney includes the funnel-shaped renal pelvis, lying within the renal sinus. The renal pelvis collects urine from the pyramids and conveys it into the ureter for passage to the urinary bladder. Let's take a look at the structure of a nephron in greater detail. Here you see a juxtamedullary nephron. The nephron is the structural and functional unit of the kidneys. It consists of a specialized tubular structure and closely associated blood vessels. Let's trace the blood flow to and from a nephron. Recall that blood entering the kidney through the renal artery flows first into the segmental arteries. From there, it enters the interlobar arteries, the arcuate arteries, the small cortical radiate arteries and the still smaller afferent arterioles which empty into a capillary bed called the glomerulus. Leading away from the glomerulus is the efferent arteriole. Notice that the afferent arteriole is larger in diameter than the efferent arteriole. Blood passes from the efferent arteriole into the peritubular capillaries and vasa recta. From there blood drains into the cortical radiate vein, flows into the arcuate vein and enters the Interlobar vein eventually reaching the renal vein. Let's see the nephron's tubular structure. The tubular structure of the nephron is relatively complex. Let's simplify the diagram further. The expanded cup-shaped end of the tubule surrounding the glomerulus is called the Glomerular, or Bowman's capsule. Water and solutes pass from the blood into the Glomerular capsule and then flow into the proximal convoluted tubule, or PCT. After many loops and convolutions, the tubule straightens out and fluid flows down the descending, or thin segment, of the nephron loop into the medullary region and then up the ascending, or thick segment, back into the cortical region. From the nephron loop, the fluid then enters the twists and turns of the distal convoluted tubule, or DCT, eventually emptying into a cortical collecting duct. This duct extends into the medulla, forming the medullary collecting duct, which carries the urine through the tubules of the renal pyramids to the renal pelvis. The next few parts of this lesson will follow the flow of fluid through the nephron and discuss the unique characteristics of the specialized cells in each segment. Let's start with the Glomerular capsule to examine this initial segment in greater detail. The glomerulus with its larger incoming afferent arteriole and smaller outgoing efferent arteriole is nested within the Glomerular capsule, something like a fist thrust into a balloon. Together, these structures are called the renal corpuscle. The visceral layer of the Glomerular capsule is made up of specialized cells called podocytes, which surround the permeable capillaries. Between the visceral and parietal layers of the capsule lies the capsular space which collects the fluid and solutes being filtered from the blood. Let's take a look at an enlarged view of a glomerular capillary. Here we see a glomerular capillary in longitudinal section.The endothelial lining shows small openings called fenestrations, which allow for the passage of water and solutes such as ions and small molecules. Let's see a view of the endothelium from outside. Now as the capillary endothelium is completed on the screen, you can see the fenestrations more clearly. Let's now see a basement membrane. The porous basement membrane encloses the capillary endothelium. Surrounding the basement membrane is a layer of podocytes. These cells have large leg-like extensions, which in turn have small fringe-like extensions called pedicels. Pedicels from adjacent areas interdigitate loosely to form spaces called filtration slits. Substances being filtered must pass first through the fenestrations, then through the basement membrane and finally through the filtration slits and into the capsular space. Together the capillary endothelium, basement membrane, and podocytes make up the filtration membrane. Let's take a look at a photomicrograph of a glomerular capillary. Here is a photomicrograph of a podocyte overlying a capillary. Extending from the podocyte cell body are leg-like extensions containing the fringe-like pedicels. Notice how these extensions and pedicels wrap around the capillary and interdigitate to form the filtration slits. This photomicrograph shows a cross-section of the filtration membrane. Starting from the top, you see a large podocyte with its nucleus and pedicels. The wide areas are portions of the capsular space. Gaps between the pedicels are the filtration slits. Next you see the basement membrane of the capillary endothelium which separates the podocyte above from the capillary with its fenestrations below. You can also see portions of two red blood cells. Let's now see an animation of filtration. Notice that the filtration membrane permits the escape of small molecules while preventing large molecules, particularly proteins, from leaving the bloodstream and passing through into the capsular space. Continuing our tour of the nephron, we will now look at the proximal convoluted tubule on the small nephron to see the cells of that region. The simple cuboidal cells of the proximal convoluted tubule are called brush border cells because of their numerous microvilli which project into the lumen of the tubule. These microvilli greatly expand the surface area of the luminal membrane adapting it well for the process of reabsorption. Tight junctions between adjacent cells permit passage of water but limit the escape of large molecules from the tubular lumen into the interstitial space. The highly folded basolateral membrane of the cells contains numerous integral proteins involved in passive or active transport of substances between the intracellular and interstitial spaces. Numerous mitochondria provide the ATP necessary for these active transport processes. The key feature of these cells is that they are highly permeable to water and many solutes. Now let's look at the thin segment of the nephron loop on the small nephron to see the cells of that region. The cells of the thin segment of the descending nephron loop are simple squamous epithelial cells. These cells lack brush borders, which reduces their surface area for reabsorption. In addition, although these cells continue to be permeable to water, they possess relatively few integral proteins that function as active transport molecules for reabsorbing solutes from the filtrate. Consequently the key feature of these cells is that they are highly permeable to water but not to solutes. Now let's look at the thick segment of the ascending nephron loop and the distal convoluted tubule on the small nephron to see the cells of that region. The epithelia of the thick ascending nephron loop and the distal convoluted tubule are similar. They are composed of cuboidal cells but they have several structural differences compared to the cells of the proximal convoluted tubule. For example these cells have fewer and smaller microvilli projecting into the lumen. In addition, the cells of the ascending limb are covered by a glycoprotein layer which along with tighter tight junctions greatly restricts the diffusion of water. The basolateral membrane is similar to that of the PCT, containing many integral proteins and closely associated mitochondria for passive and active membrane transport processes. The key feature of the cells of the ascending limb is that they are highly permeable to solutes, particularly sodium chloride but not to water. The cells of the DCT are more permeable to water than those of the ascending limb. This photomicrograph shows a cross section of a glomerulus surrounded by a glomerular capsule. It also shows several proximal convoluted tubules and a single distal convoluted tubule. The microvilli in the lumen of the proximal convoluted tubules appear fuzzy because they do not stand up well to the slide preparation process. Notice the much clearer open lumen of the DCT which is less obstructed because it has fewer microvilli. Now we will look at the DCT to see a specialized region called the juxtaglomerular apparatus. As the thick ascending nephron loop transitions into the early distal convoluted tubule, the tubule runs adjacent to the afferent and efferent arterioles. Where the cells of the arterioles and of the thick ascending nephron loop are in contact with each other, they form the monitoring structure called the juxtaglomerular apparatus. The modified smooth muscle cells of the arterioles, mainly the afferent arteriole, in this area are called granular cells. These enlarged cells serve as baroreceptors sensitive to blood pressure within the arterioles. Cells of the thick ascending segment in contact with the arterioles form the macula densa. These cells monitor and respond to changes in the sodium chloride concentration of the filtrate in the tubule. Now let's look into the cortical collecting duct on the small nephron to see the cells of this region. The cuboidal cells of the cortical collecting duct fall into two distinct functional types, principal cells and intercalated cells. The more numerous principal cells have few microvilli and basolateral folds. These specialized cells respond to certain hormones that regulate the cell's permeability to water and solutes, specifically sodium and potassium ions. When the acidity of the body increases, the intercalated cells secrete hydrogen ions into the urine to restore the acid base balance of the body. The key feature of principal cells is that their permeability to water and solutes is physiologically regulated by hormones. The key feature of intercalated cells is their secretion of hydrogen ions for acid base balancing. Now let's take a look at the medullary collecting duct on the small nephron. Principal cells of the medullary collecting duct are mostly cuboidal in shape. The luminal and basolateral membranes are relatively smooth and the cells possess few mitochondria. The permeability of these cells to water and urea is hormonally regulated as the fluid passes through this region. The key feature of these cells is their hormonally regulated permeability to water and urea. These photomicrographs show a longitudinal section and a cross-section of collecting ducts. Notice that the ducts are composed of cuboidal cells. Also notice that the lumen of the collecting duct, shown in cross-section, is much larger than the lumens of the adjacent thick ascending tubules. This reflects the volume of fluid the collecting ducts contain as they gather the fluid from many nephrons. The longitudinal section here shows two ducts joining to form a larger duct. Here is a summary of what we've covered The urinary system is composed of the kidneys, ureters, urinary bladder, and urethra. The kidney is composed of three regions: the renal cortex, medulla and pelvis. The functional unit of the kidney, the nephron, is composed of a tubular portion and associated blood vessels. Each region of the tubular portion of the nephron depends on the unique features of its epithelial cells to carry out its function.
Table of contents
- 1. Introduction to Anatomy & Physiology5h 40m
- What is Anatomy & Physiology?20m
- Levels of Organization13m
- Variation in Anatomy & Physiology12m
- Introduction to Organ Systems27m
- Homeostasis9m
- Feedback Loops11m
- Feedback Loops: Negative Feedback19m
- Feedback Loops: Positive Feedback11m
- Anatomical Position7m
- Introduction to Directional Terms3m
- Directional Terms: Up and Down9m
- Directional Terms: Front and Back6m
- Directional Terms: Body Sides12m
- Directional Terms: Limbs6m
- Directional Terms: Depth Within the Body4m
- Introduction to Anatomical Terms for Body Regions3m
- Anatomical Terms for the Head and Neck8m
- Anatomical Terms for the Front of the Trunk8m
- Anatomical Terms for the Back9m
- Anatomical Terms for the Arm and Hand9m
- Anatomical Terms for the Leg and Foot15m
- Review- Using Anatomical Terms and Directions12m
- Abdominopelvic Quadrants and Regions19m
- Anatomical Planes & Sections17m
- Organization of the Body: Body Cavities13m
- Organization of the Body: Serous Membranes14m
- Organization of the Body: Serous Membrane Locations8m
- Organization of the Body: Thoracic Cavity8m
- Organization of the Body: Abdominopelvic Cavity12m
- 2. Cell Chemistry & Cell Components12h 37m
- Atoms- Smallest Unit of Matter57m
- Isotopes39m
- Introduction to Chemical Bonding19m
- Covalent Bonds40m
- Noncovalent Bonds5m
- Ionic Bonding37m
- Hydrogen Bonding19m
- Introduction to Water7m
- Properties of Water- Cohesion and Adhesion7m
- Properties of Water- Density8m
- Properties of Water- Thermal14m
- Properties of Water- The Universal Solvent17m
- Acids and Bases12m
- pH Scale21m
- Carbon8m
- Functional Groups9m
- Introduction to Biomolecules2m
- Monomers & Polymers11m
- Carbohydrates23m
- Proteins25m
- Nucleic Acids34m
- Lipids28m
- Microscopes10m
- Prokaryotic & Eukaryotic Cells26m
- Introduction to Eukaryotic Organelles16m
- Endomembrane System: Protein Secretion34m
- Endomembrane System: Digestive Organelles15m
- Mitochondria & Chloroplasts21m
- Endosymbiotic Theory10m
- Introduction to the Cytoskeleton10m
- Cell Junctions8m
- Biological Membranes10m
- Types of Membrane Proteins7m
- Concentration Gradients and Diffusion9m
- Introduction to Membrane Transport14m
- Passive vs. Active Transport13m
- Osmosis33m
- Simple and Facilitated Diffusion17m
- Active Transport30m
- Endocytosis and Exocytosis15m
- 3. Energy & Cell Processes10h 7m
- Introduction to Energy15m
- Laws of Thermodynamics15m
- Chemical Reactions9m
- ATP20m
- Enzymes14m
- Enzyme Activation Energy9m
- Enzyme Binding Factors9m
- Enzyme Inhibition10m
- Introduction to Metabolism8m
- Redox Reactions15m
- Introduction to Cellular Respiration22m
- Types of Phosphorylation11m
- Glycolysis19m
- Pyruvate Oxidation8m
- Krebs Cycle16m
- Electron Transport Chain14m
- Chemiosmosis7m
- Review of Aerobic Cellular Respiration19m
- Fermentation & Anaerobic Respiration23m
- Introduction to Cell Division22m
- Organization of DNA in the Cell17m
- Introduction to the Cell Cycle7m
- Interphase18m
- Phases of Mitosis48m
- Cytokinesis16m
- Cell Cycle Regulation18m
- Review of the Cell Cycle7m
- Cancer13m
- Introduction to DNA Replication22m
- DNA Repair7m
- Central Dogma7m
- Introduction to Transcription20m
- Steps of Transcription19m
- Genetic Code25m
- Introduction to Translation30m
- Steps of Translation23m
- Post-Translational Modification6m
- 4. Tissues & Histology10h 3m
- Introduction to Tissues & Histology16m
- Introduction to Epithelial Tissue24m
- Characteristics of Epithelial Tissue37m
- Structural Naming of Epithelial Tissue19m
- Simple Epithelial Tissues1h 2m
- Stratified Epithelial Tissues55m
- Identifying Types of Epithelial Tissue32m
- Glandular Epithelial Tissue26m
- Introduction to Connective Tissue36m
- Classes of Connective Tissue8m
- Introduction to Connective Tissue Proper40m
- Connective Tissue Proper: Loose Connective Tissue56m
- Connective Tissue Proper: Dense Connective Tissue49m
- Specialized Connective Tissue: Cartilage44m
- Specialized Connective Tissue: Bone12m
- Specialized Connective Tissue: Blood9m
- Introduction to Muscle Tissue7m
- Types of Muscle Tissue45m
- Introduction to Nervous Tissue8m
- Nervous Tissue: The Neuron8m
- 5. Integumentary System2h 20m
- 6. Bones & Skeletal Tissue2h 16m
- An Introduction to Bone and Skeletal Tissue18m
- Gross Anatomy of Bone: Compact and Spongy Bone7m
- Gross Anatomy of Bone: Periosteum and Endosteum11m
- Gross Anatomy of Bone: Bone Marrow8m
- Gross Anatomy of Bone: Short, Flat, and Irregular Bones5m
- Gross Anatomy of Bones - Structure of a Long Bone23m
- Microscopic Anatomy of Bones - Bone Matrix9m
- Microscopic Anatomy of Bones - Bone Cells25m
- Microscopic Anatomy of Bones - The Osteon17m
- Microscopic Anatomy of Bones - Trabeculae9m
- 7. The Skeletal System2h 35m
- 8. Joints2h 17m
- 9. Muscle Tissue2h 33m
- 10. Muscles1h 11m
- 11. Nervous Tissue and Nervous System1h 35m
- 12. The Central Nervous System1h 6m
- 13. The Peripheral Nervous System1h 26m
- Introduction to the Peripheral Nervous System5m
- Organization of Sensory Pathways16m
- Introduction to Sensory Receptors5m
- Sensory Receptor Classification by Modality6m
- Sensory Receptor Classification by Location8m
- Proprioceptors7m
- Adaptation of Sensory Receptors8m
- Introduction to Reflex Arcs13m
- Reflex Arcs15m
- 14. The Autonomic Nervous System1h 38m
- 15. The Special Senses2h 41m
- 16. The Endocrine System2h 48m
- 17. The Blood1h 22m
- 18. The Heart1h 42m
- 19. The Blood Vessels3h 35m
- 20. The Lymphatic System3h 16m
- 21. The Immune System14h 37m
- Introduction to the Immune System10m
- Introduction to Innate Immunity17m
- Introduction to First-Line Defenses5m
- Physical Barriers in First-Line Defenses: Skin13m
- Physical Barriers in First-Line Defenses: Mucous Membrane9m
- First-Line Defenses: Chemical Barriers24m
- First-Line Defenses: Normal Microbiota7m
- Introduction to Cells of the Immune System15m
- Cells of the Immune System: Granulocytes28m
- Cells of the Immune System: Agranulocytes26m
- Introduction to Cell Communication5m
- Cell Communication: Surface Receptors & Adhesion Molecules16m
- Cell Communication: Cytokines27m
- Pattern Recognition Receptors (PRRs)48m
- Introduction to the Complement System24m
- Activation Pathways of the Complement System23m
- Effects of the Complement System23m
- Review of the Complement System13m
- Phagocytosis17m
- Introduction to Inflammation18m
- Steps of the Inflammatory Response28m
- Fever8m
- Interferon Response25m
- Review Map of Innate Immunity
- Introduction to Adaptive Immunity32m
- Antigens12m
- Introduction to T Lymphocytes38m
- Major Histocompatibility Complex Molecules20m
- Activation of T Lymphocytes21m
- Functions of T Lymphocytes25m
- Review of Cytotoxic vs Helper T Cells13m
- Introduction to B Lymphocytes27m
- Antibodies14m
- Classes of Antibodies35m
- Outcomes of Antibody Binding to Antigen15m
- T Dependent & T Independent Antigens21m
- Clonal Selection20m
- Antibody Class Switching17m
- Affinity Maturation14m
- Primary and Secondary Response of Adaptive Immunity21m
- Immune Tolerance28m
- Regulatory T Cells10m
- Natural Killer Cells16m
- Review of Adaptive Immunity25m
- 22. The Respiratory System3h 20m
- 23. The Digestive System2h 5m
- 24. Metabolism and Nutrition4h 0m
- Essential Amino Acids5m
- Lipid Vitamins19m
- Cellular Respiration: Redox Reactions15m
- Introduction to Cellular Respiration22m
- Cellular Respiration: Types of Phosphorylation14m
- Cellular Respiration: Glycolysis19m
- Cellular Respiration: Pyruvate Oxidation8m
- Cellular Respiration: Krebs Cycle16m
- Cellular Respiration: Electron Transport Chain14m
- Cellular Respiration: Chemiosmosis7m
- Review of Aerobic Cellular Respiration18m
- Fermentation & Anaerobic Respiration23m
- Gluconeogenesis16m
- Fatty Acid Oxidation20m
- Amino Acid Oxidation17m
- 25. The Urinary System2h 39m
- 26. Fluid and Electrolyte Balance, Acid Base Balance Coming soon
- 27. The Reproductive System2h 5m
- 28. Human Development1h 21m
- 29. Heredity Coming soon
25. The Urinary System
The Kidneys
Video duration:
17mPlay a video:
Related Videos
Related Practice